Abstract
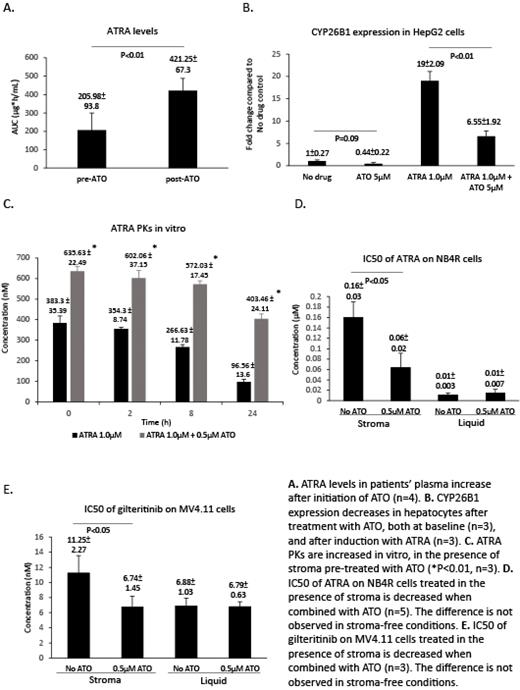
Eliminating minimal residual disease (MRD) in order to prevent relapse is an unmet need in acute myeloid leukemia (AML). One of the success stories is acute promyelocytic leukemia (APL), a unique subtype of AML. The use of arsenic trioxide (ATO) in combination with all-trans retinoic acid (ATRA) has essentially eliminated disease relapse (<1% ATRA+ATO vs. ~18% ATRA+ chemotherapy - NEJM (2013), 369(2), 111-121). This is even more impressive as neither agent alone results in significant cure of patients with APL. In fact, single agent ATRA induces remission without cure due to bone marrow stroma expression of CYP26 enzymes (PloS one (2015), 10(6), e0127790), which are induced by ATRA, inactivate retinoids and protect APL MRD (Leukemia (2020), 34(11), 3077-3081). While ATO may synergize with ATRA by restoring PML nuclear bodies (Nature medicine (2014), 20(2), 167-174) and rescuing RAR-α dependent transcription (Nature reviews. Cancer (2018), 18(2), 117-127) in the bulk of the APL tumor cells, it is unclear how these mechanisms contribute to elimination of MRD, particularly given the hypothesized lack of ATRA in the bone marrow niche. It was previously reported that combination of ATRA with ATO may be associated with high incidence of transaminitis and headaches (NEJM (2013), 369(2), 111-121). Since these may be clinical signs of ATRA toxicity, we investigated if addition of ATO changes the pharmacokinetics (PKs) of ATRA in patients with APL. We determined the area under the plasma concentration versus time curve (AUC) for ATRA in patients suspected of APL and treated with single agent ATRA ("preATO") and in the same patients after the diagnoses of APL was confirmed and the patients received ATO ("postATO"). Even though ATRA should have an expected drop in AUC during the first 3-4 days of therapy (JPET (2017), 361(2), 246-258), addition of ATO resulted in improved ATRA PKs (Figure A). Since ATRA levels are mainly controlled by clearance via hepatic CYP26s, we tested if treatment with ATO changes the levels of CYP26 or its induction by ATRA. We found that exposure to ATO decreases both baseline and ATRA-induced upregulation of CYP26B1 in HepG2 cells (Figure B). Similarly, ATO decreases CYP26B1 levels in human bone marrow derived mesenchymal stroma cells (MSCs) at baseline (21%±7% of NO ATO control, n=3, p<0.01) and after ATRA-induced upregulation (66%±14% of ATRA only control, n=3, p<0.01). These changes resulted in improved ATRA PKs in vitro in the presence of bone marrow MSCs (Figure C). Next, we used NB4-EvAsR cells (NB4R), ATO-resistant APL cells to test if ATO-induced improvement of MSC-dependent ATRA PKs may contribute to elimination of APL MRD. We found that ATO sensitizes NB4R to ATRA in the presence of BM MSCs but not in stroma free conditions (Figure D). ATO had no effect on ATRA-induced differentiation of NB4R in the presence of CYP26B1 knockout stroma (this stroma offers no protection from ATRA) or if stroma expresses CYP26B1 under the control of a viral promoter and thus, resistant to ATO downregulation. This data suggest that ATO-induced changes of BM MSC expression of CYP26 may contribute to elimination of MRD in APL. Stromal CYP26 protects not only APL but also non-APL AML cells from retinoids (Leukemia (2020), 34(11), 3077-3081). Retinoids are synergistic with FLT3 inhibitors to eliminate mutant FLT3 AML cells (Blood (2016), 127(23), 2867-2878) and stromal CYP26 breaks this synergism (Blood (2015) 126 (23): 790). We tested if ATO sensitizes mutant FLT3 AML cells, MV4;11 to gilteritinib in the presence of BM MSCs. For this, we derived MV4.11 cells resistant to ATO (MV4.11R) via long term exposure to increasing concentration of ATO. As seen with NB4R, ATO treatment synergizes with gilteritinib to decrease the IC50 of gilteritinib against the clonogenic activity of MV4.11R in the presence of stroma but not in stroma free conditions (Figure E). In an effort to fully explore the translational potential of these findings, we are currently investigating the mechanism by which ATO changes CYP26 levels.
Taken together these findings support a model in which ATO changes the bone marrow niche and it's ability to metabolize retinoids and thus, sensitizes MRD in AML to targeted therapy.
Mathews: Christian Medical College: Patents & Royalties: US 2020/0345770 A1 - Pub.Date Nov.5, 2020; AML: Other: Co-Inventor. Ghiaur: Syros Pharmaceuticals: Consultancy; Menarini Richerche: Research Funding.